In the June Network Bulletin from UnitedHealthcare, I came across an article discussing the proper way to file a secondary claim when Medicare is primary. Even though the information was not new, I thought it might be helpful to go back through the 3 ways you can file secondary claims.
Billing Note: CMS has posted a recommendation on proper billing when a commercial payer is secondary.
 Medicare Crossover Claims
Medicare Crossover Claims
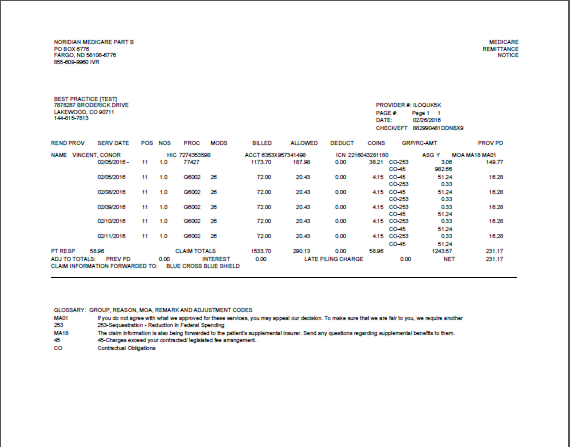
As UHC pointed out, many times Medicare sends the crossover claim directly to most major commercial payers and Medicaid programs also. The biller can determine if this has been done by checking the Medicare explanation of benefits (EOB). Any claims that have been electronically crossed over to a secondary payer with have Remittance Advice Remark Code (RARC) MA18 indicated on the EOB.
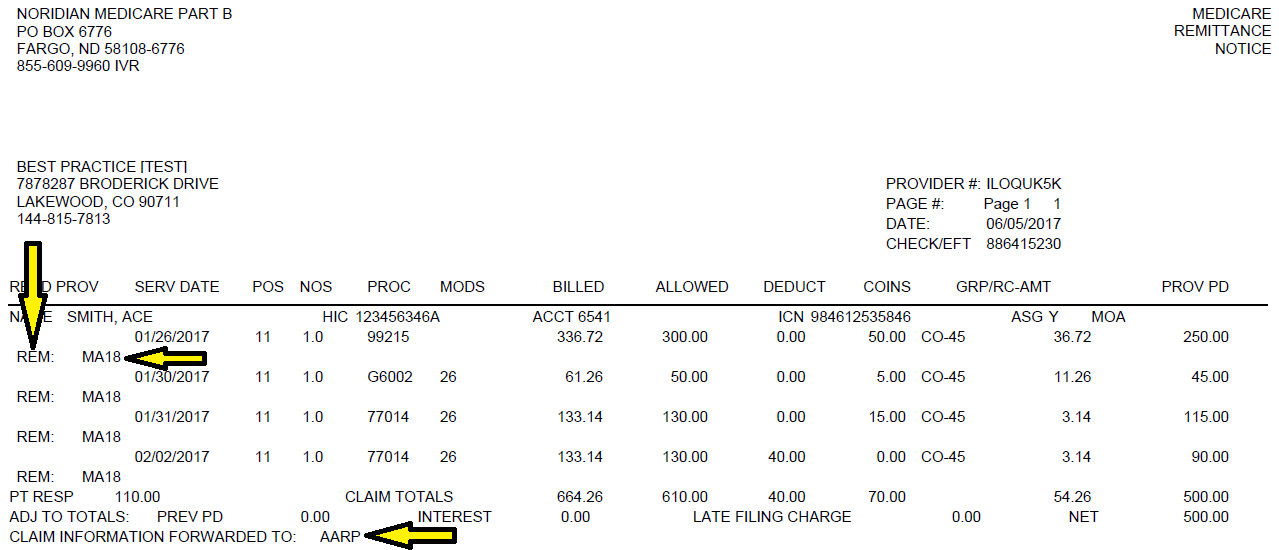
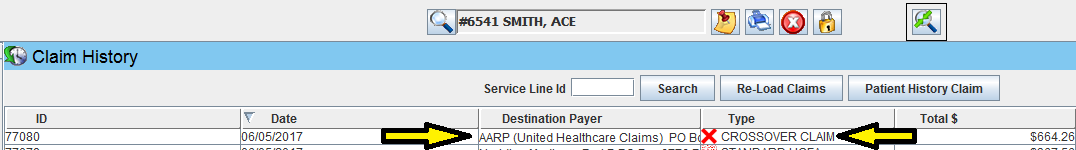
 Iridium Suite Practice Management Software by Shavara, Inc. will indicate a crossover claim automatically when the data is included in the 835 electronic remittance advice (ERA) data file. This will prevent the needless filing a secondary claim by the user.
Iridium Suite Practice Management Software by Shavara, Inc. will indicate a crossover claim automatically when the data is included in the 835 electronic remittance advice (ERA) data file. This will prevent the needless filing a secondary claim by the user.
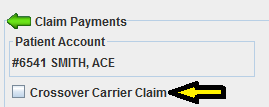
On the rare occasion a Medicare payment requires manual posting, the user can easily indicate when the claim was crossed over to the secondary right in the payment posting screen:
 Electronic Coordination of Benefits Claims
Electronic Coordination of Benefits Claims
In this age of technology, many payers have enabled their claims processing systems to receive and process secondary claims electronically. This means that in addition to a standard 837 claim data file, a data file that includes the primary payer’s information is included in the transmission.
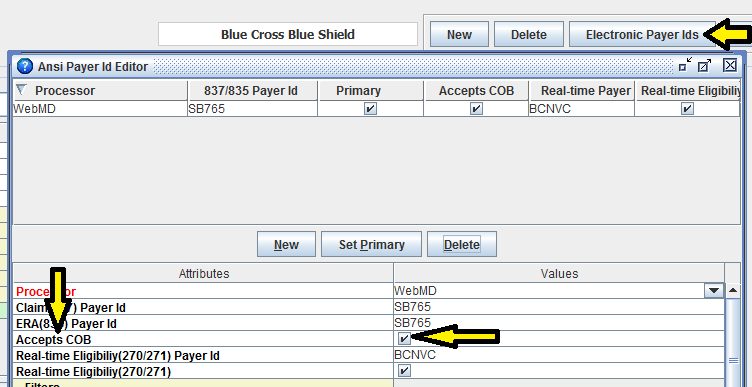
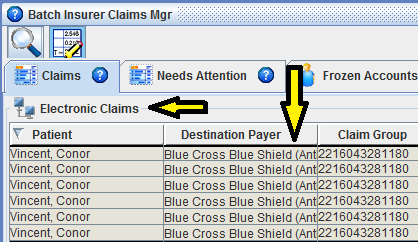
In Iridium Suite, you can easily see if a payer accepts coordination of benefits (COB) claims electronically:
The medical billing software automatically puts the secondary claim into the electronic claims batch for quick submission to the payer:
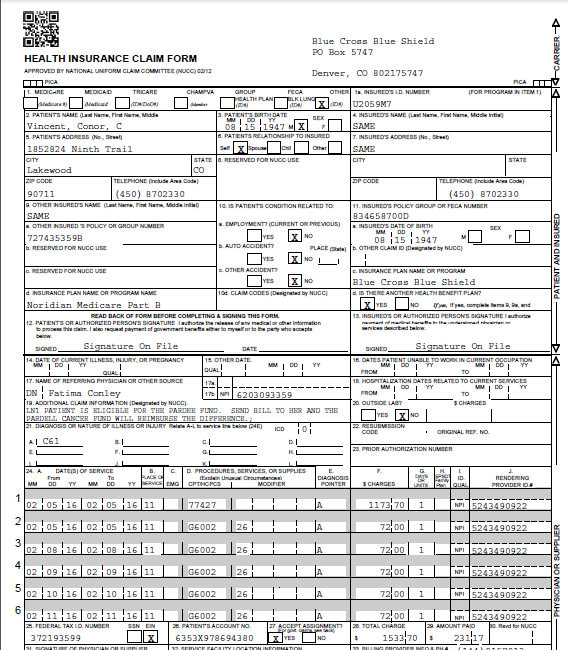
Secondary Paper Claims
This last way to file secondary claims is the least convenient. It requires the biller to manually print the claim and attach a copy of the standard paper remittance (SPR).
Iridium Suite makes this process a little more streamlined by automatically creating the SPR and putting in the paper claims batch adjacent to the claim form.
Whether your secondary claim is filed by method 1, 2, or 3 it is imperative for proper revenue cycle management to monitor Accounts Receivables for secondary payers regularly (at least once a month). The Iridium Suite Accounts Receivables module facilitates this process.


