A Medical Practice is a unique business in many ways, but it is still a business and must be treated as such. Checking the health of your practice is similar to checking the health of your patients. In this three part series, we will look at these Vital Signs, pulse, blood pressure and temperature, to help you assess the financial well-being of your medical practice.
In Part 1, we addressed the pulse of your practice: trends in new patient statistics and physician referrals. If you missed Part 1, please select this link: Check the Vital Signs of Your Medical Practice-Part 1
For Part 2, let’s check that Blood Pressure- 
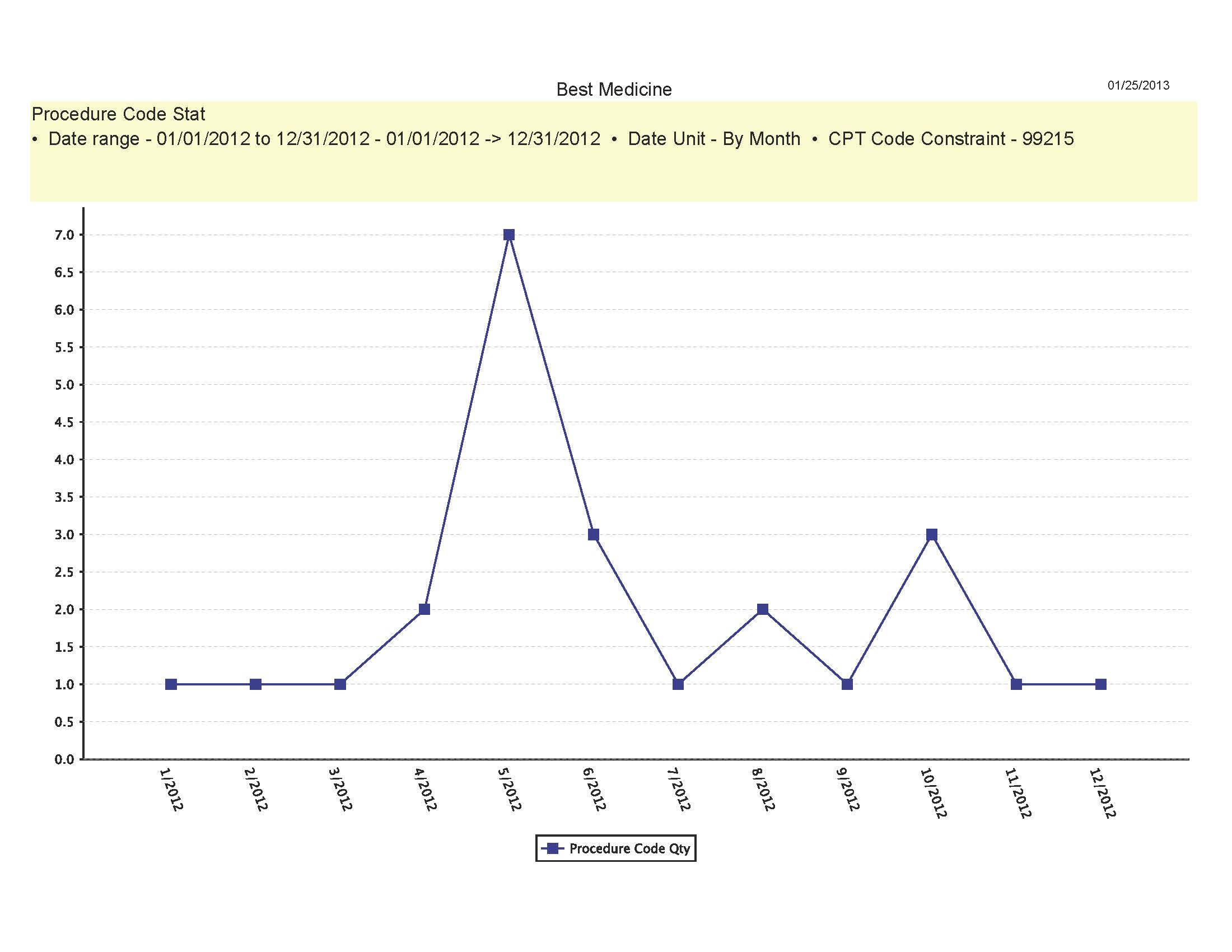
Are the numbers of services you bill increasing, decreasing, or staying the same?
Depending on your type of medical practice, you could expect to see one or two procedure codes billed per patient visit or for some specialties like Radiation Oncology, you may bill 10 procedure codes per visit. In either case, reviewing reports that show month-to-month statistics can allow you to recognize anomalies in your billing patterns. Sharp declines in a certain procedure may indicate forgotten or missed coding opportunities and therefore missed revenue. Many payers have time filing limits from the date of service. They can range from 60 days to one year. A regular review for missed charges will enable to meet those filing limits and collect on all of your rendered services. If your report showed an unexpected procedure or an unusually high number of a certain procedure was billed, you will be able to audit the medical record(s) for appropriate documentation. If billing errors are discovered, you can get ahead of an insurance audit by quickly refunding any payments received for these non-provided services. Keeping yourself in the good graces of your payers is always important.
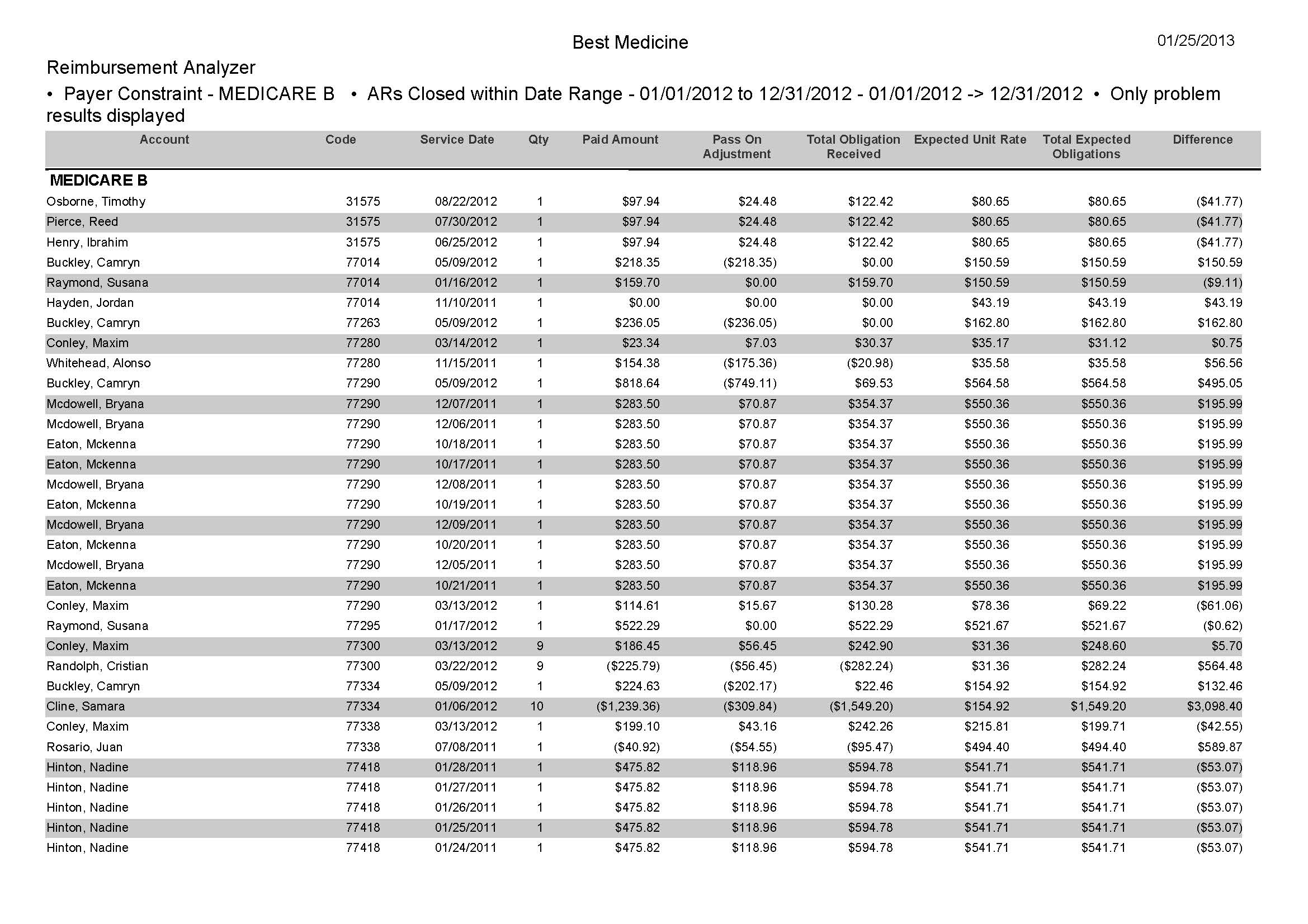
Is your claim reimbursement in line with your contracted fees?
This type of analysis is invaluable to any medical practice. Once you have signed on that dotted line with the payer, you are wise to ensure that you are receiving the proper reimbursement based on the agreed upon contractual rates. In the daily whirlwind of activity in the medical office, office staff seldom has the time to comb over the detail of every paid line item. A monthly report that compares the payments received to the payer’s fee schedule will indicate payments that are below (as well as above) the payers contracted fees. Payments that are below should immediately prompt a call the Provider Relations Department. For payments above the contracted fees, research has to be done on the accuracy of the fee schedule you are using, for instance, perhaps the payer has updated its schedule and you have not. This type of report could also make you aware of overpayments. If those are pre-emptively refunded to the payer, it will show your practice to be following proper procedures in the eyes of the payer.
These two reports are just a small sampling of the extensive selection of practice management reporting options built into the Report Center module of Iridium Suite Medical Billing Software.
Be sure to watch for the upcoming publication of Part 3: Temperature.



