As a medical biller one of the constant issues we encounter is out of date or inaccurate insurance coverage information. It delays payments and causes a lot work for office staff. I thought it would be helpful for our Iridium Suite users if I created a “cheat sheet” of the 3 common scenarios.

REMEMBER: Most questions you may have about any functions in the Iridium Suite medical billing software can be answered by accessing the online Help Manual. A simple click on any ![]() will take you there!
will take you there!
Scenario 1:
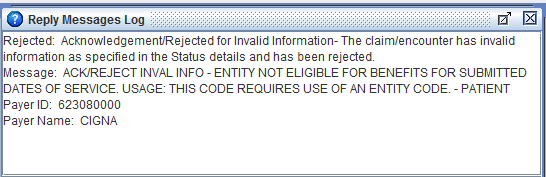
- You have billed the primary payer on file for the patient via electronic claim.
- You received an electronic claim rejection via the Electronic Claims Queue. The message may be: patient coverage is terminated, not eligible, OR service covered by another provider.
How to resolve:
- Contact the patient to update current payer policy information.
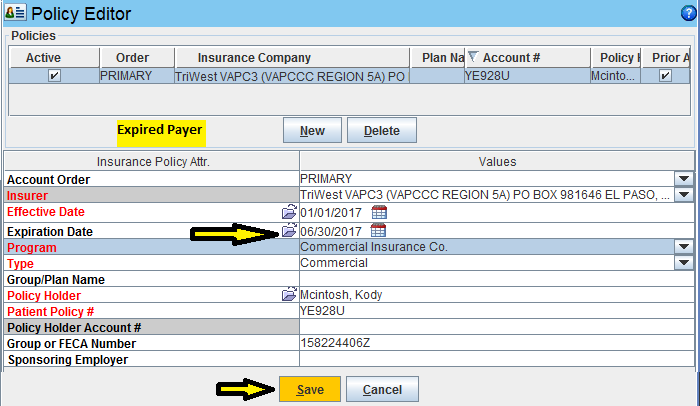
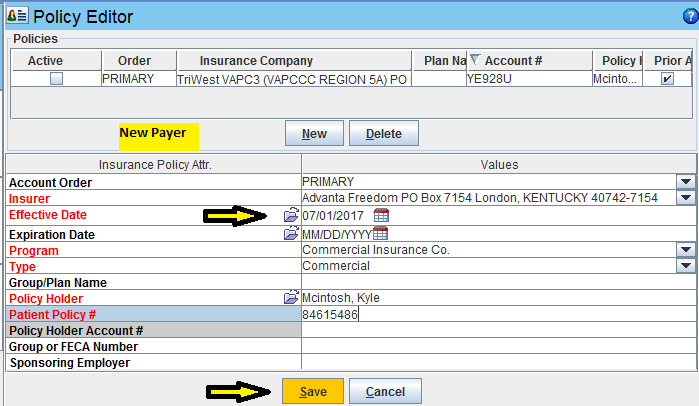
- Update the Insurance Policy Manager with the payer information.
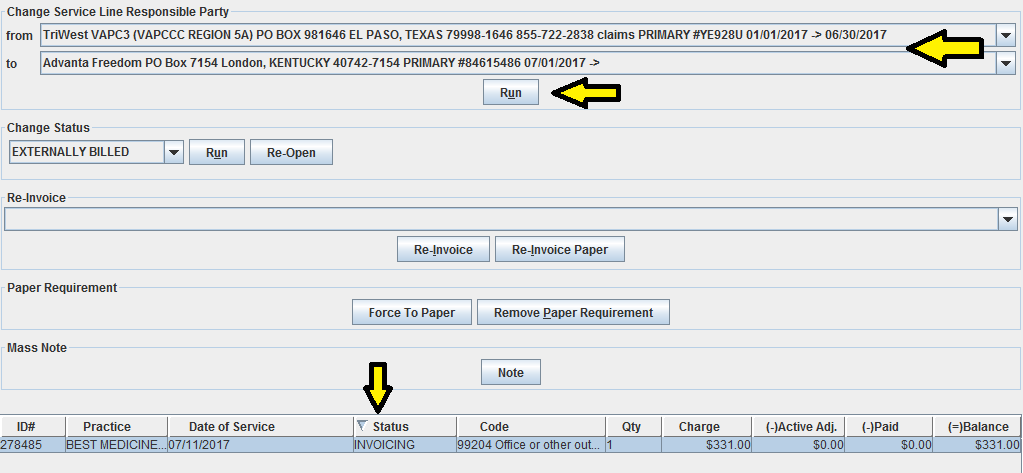
- Go to the Service Line Repair Tool. Select the payers to transfer from and to, select the applicable service lines, and select Run. This moves the Service Line Responsibility to the appropriate payer.
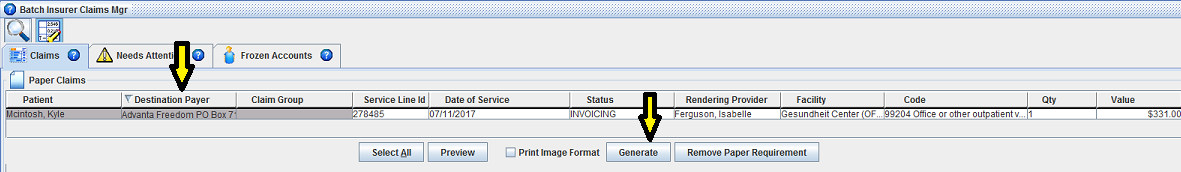
- Go to the Batch Insurer Claims, search, select and generate applicable service lines. Claim(s) will now go to new payer.
NOT AN IRIDIUM SUITE CUSTOMER (YET)? You can be. Set up your  practice management software demo today.
practice management software demo today.
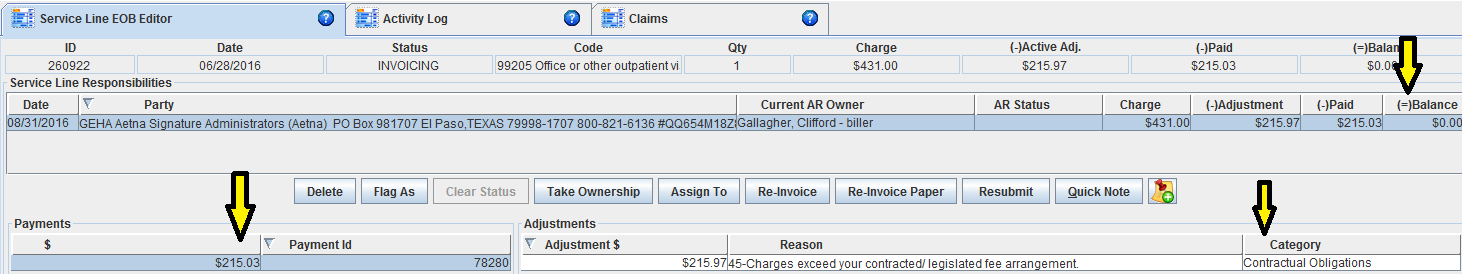
Scenario 2:
- You have billed the primary payer on file for the patient via electronic or paper claim.
- You received a denial from the payer that you find when performing routine Accounts Receivable audit.
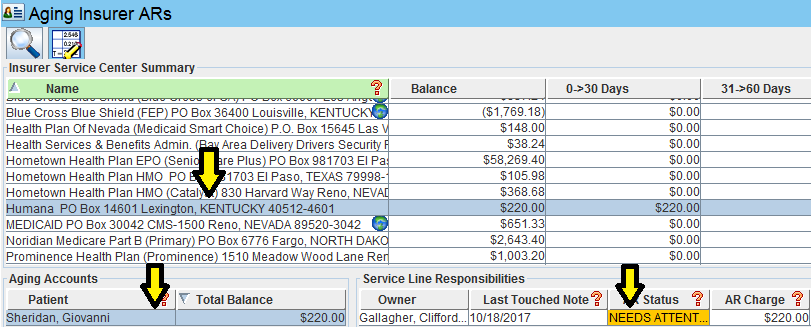
- The Reason Code may indicate: patient coverage is terminated, not eligible OR service covered by another payer.
How to resolve:
- Contact the patient to update current payer policy information.
- Update the Insurance Policy Manager with the payer information.
- Go to the Batch Insurer Claims, search, select and generate applicable service lines. Claim(s) will now go to new payer.
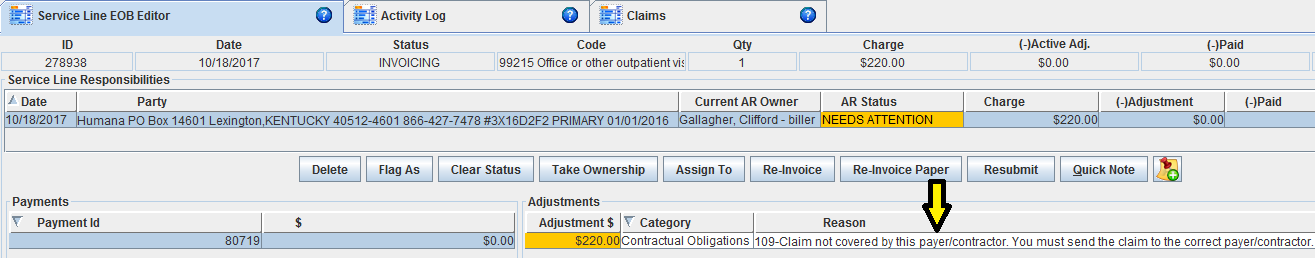
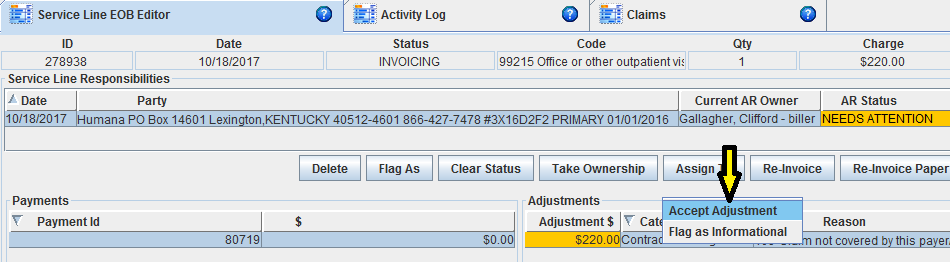
- Go to the Service Lines screen and select the Needs Attention service line. Mark the denial adjustment as Accepted.

As mentioned above, the online Help Manual is a terrific resource for users.
Occasionally though it might be advantageous for staff to get a medical billing software training refresher or maybe new users need more in-depth training that can be done by you staff.
Scenario 3:
- You have billed the primary payer on file for the patient via electronic or paper claim.
- You received a payment from the payer.
- You received updated payer information indicating the incorrect payer was billed.
How to resolve:
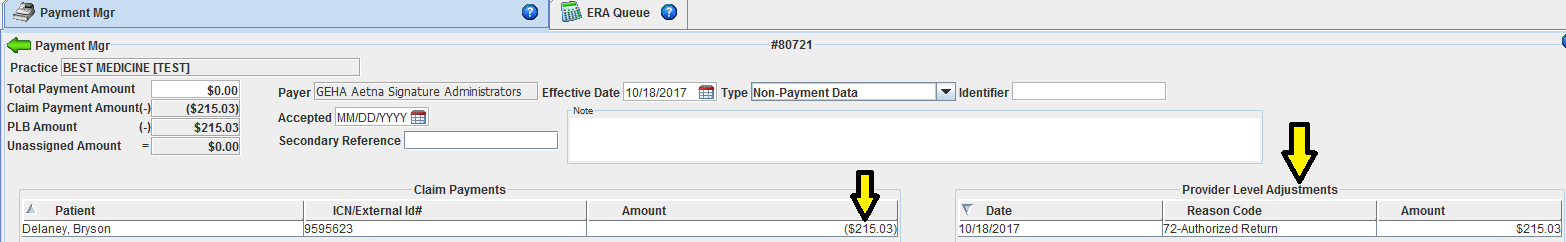
- The reversal of the payment is posted.
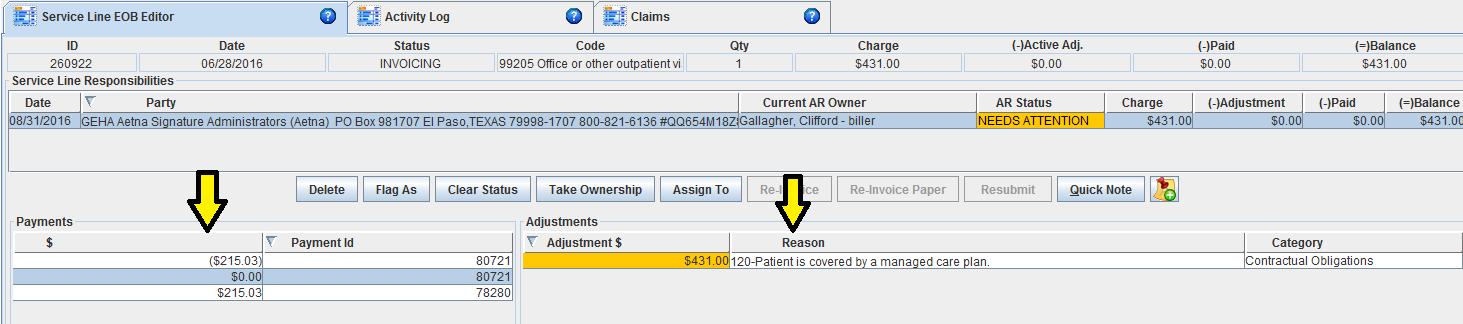
- This creates an Unassigned Payment in the Payment Manager. You use that payment to indicate the payer refund.
- Contact the patient to update current payer policy information.
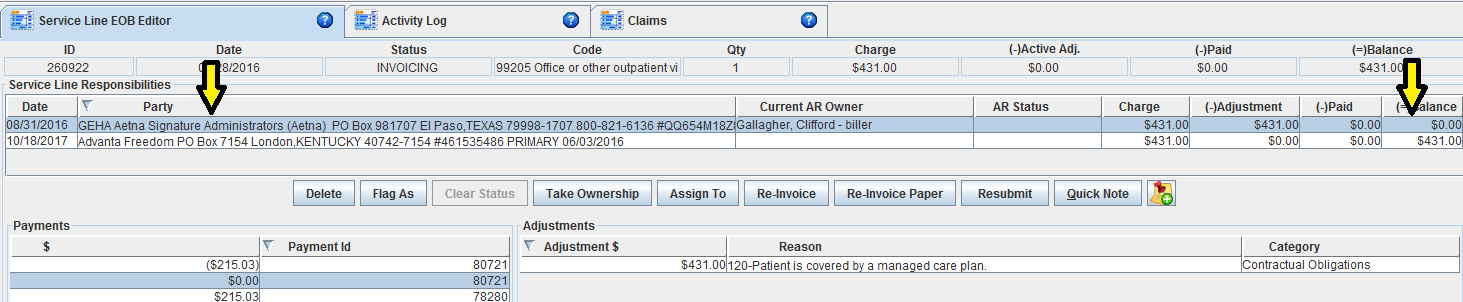
- Update the Insurance Policy Manager with the payer information.
- Go to the Batch Insurer Claims, search, select and generate applicable service lines. Claim(s) will now go to new payer.
- Go to the Service Lines screen and select the Needs Attention service line. Mark the denial adjustment as Accepted. You will see the incorrect payer balance at $0 and the new correct payer balance equal to the charge amount.
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin-top:0in;
mso-para-margin-right:0in;
mso-para-margin-bottom:10.0pt;
mso-para-margin-left:0in;
line-height:115%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:”Calibri”,”sans-serif”;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}

Find MORE billing hints, and healthcare infographics posted in our Medical Billing Blog!


