|
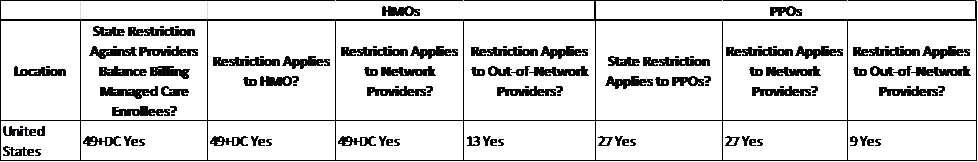
I recently read a story on an emergency plastic surgeon who was fined $562,000 and sentenced to 5 days in jail by the Los Angeles Superior Court. The offense: inappropriately billing patients for the balances disputed with health plans for their ED care. Find article here: http://www.the-leader.com/article/20140122/NEWS/140129904 49 states and the District of Columbia have addressed the issue of Managed Care Balance Billing. Some jurisdictions have more regulations than others. |
 |
A complete table with details has been published by The Henry J. Kaiser Family Foundation.
In summary:
Here are the Do’s and Don’ts of Balance Billing:
|
Do: Know the rules for your service location. Don’t: Assume that your entire billing staff is aware of the rules. Do: Know your payer contracts. Don’t: Assume that patients know if you are in-network or not. Do: Initiate good office practices for checking patient network coverage prior to providing services. Don’t: Rely on patient’s to understand their benefits. Do: Provide the best effort in informing patients of expected out of pocket expenses. Don’t: Say “You signed the form, so we can bill you whatever we want” to your patients. Do: Ensure that staff is especially mindful when generating a patient bill for providing a service in the Emergency Department, to an inpatient, or for a surgical procedure. Don’t: Assume your name or practice name on a bill is familiar to a patient. |
|
 |
As many people are becoming newly insured through the Health Insurance Exchange (HIX) plans created as part of the Affordable Care Act (ACA). The number of patients you will encounter with Managed Care policies will be increasingly common. Having an established and fair billing policy will be even more crucial to your financial success and avoiding legal trouble as well. |


