Yesterday was the somewhat official ‘Back to the Future’ Day. In the second installment of the franchise, character Marty McFly travels from 1985 to the future date of October 21, 2015.
Some of the technological advances are familiar products to us today: big screen TVs, virtual reality goggles, and FaceTime. Some are not yet reality: hoverboards, self-lacing shoes and flying cars.
It made me think about medical billing practices from 1985 compared to those of today.
Patient Appointment Scheduling
1985 – Scheduling required flipping from page to page in the paper appointment book. Typically there was a cheat sheet for the scheduler with suggestions of time blocking or available days based on the type of appointment needed.
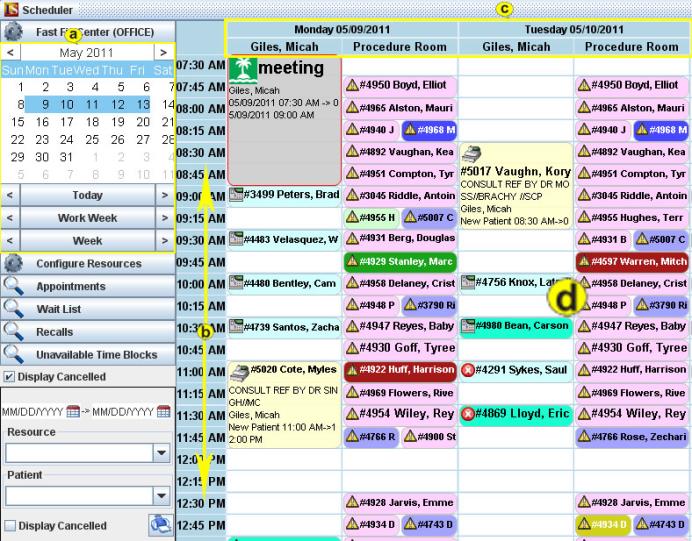
2015 – Electronic scheduling programs are customized for the practice with time blocks set for specific procedures and clinical resources.
With a couple of mouse clicks the scheduler can access a variety of available time slots and present the patient with the options.
The appointment is “linked” to the patient record with no need to making any extra notes of contact #’s etc. There are even automated appointment reminders via phone and/or email.
Confirming Patient Eligibility and Benefits
1985 – Front desk personnel would copy the patient insurance card(s) and then have to spend countless hours on the phone getting the elegibility and benefit information.

2015 – Insurance cards can be scanned and stored in the EMR.
The best practice software have built-in Real Time Eligibility functionality.
Inquires are sent via internet directly to the payers with immediate responses.
Office staff can know within seconds the status of the policy and benefit details.
Charge Capture and Claim Submittal
1985 – Paper superbills are attached to the patient charts, completed by the provider, then hopefully make their way to the biller for manual entry onto the paper claim form. Paper claim forms are mailed to the payer for processing.

2015 – Code are captured in the EMR and then are exported into billing system for electronic submission.
This is done through the standard HL7 format.
An entire days billing can be completed in just minutes.
Data like patient demographics can also be exported to the EMR to seed that data after running the RTE.
Claim Processing, Payments and Posting Remittances
1985 – Paper claims are manually processed by the payer, remittance advices are printed and paper checks are issued. Claims turn around time is typically 45 to 60 days. This has definite implications on the practice cash flow.
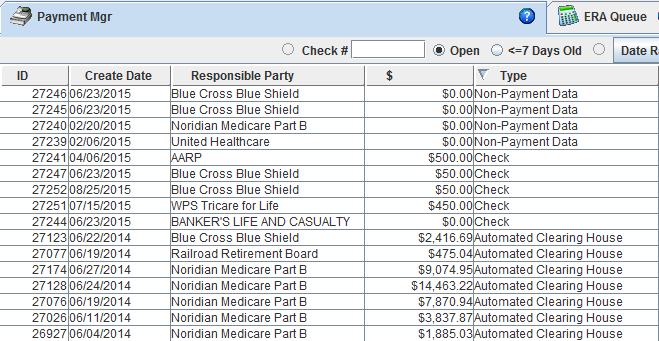
2015 – Electronic claims are processed quickly,
The electronic remittances are transmitted directly into the medical coding software.
Electronic funds transfer payments are sent directly to the practice bank account.
Often this entire cycle only takes 7 – 10 business days.
A great improvement on the cash flow.
The technological advances in the medical billing industry have given us many tools that improve our
ability to efficiently and successfully manage our medical billing business.
Find out more about our product, Iridium Suite.


